
Interesting finding by my PhD student Ashwin Mak in J Med Virol: onlinelibrary.wiley.com/doi/10.1002/... 1/6
Interesting finding by my PhD student Ashwin Mak in J Med Virol: onlinelibrary.wiley.com/doi/10.1002/... 1/6
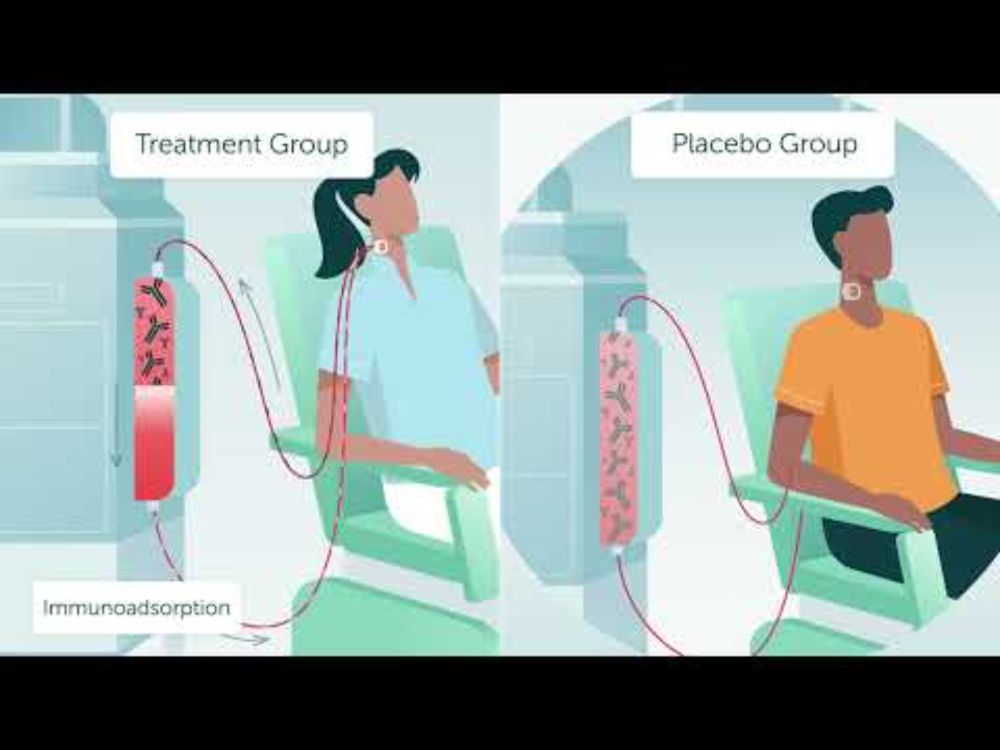
www.youtube.com/watch?v=k4m4...

www.youtube.com/watch?v=k4m4...


(1/3)
(1/3)

