






doi.org/10.1016/j.kint.2025.05.033
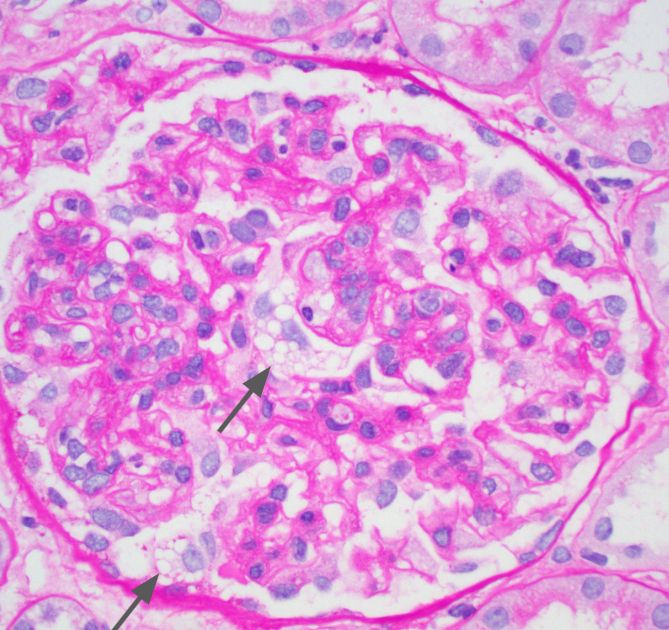
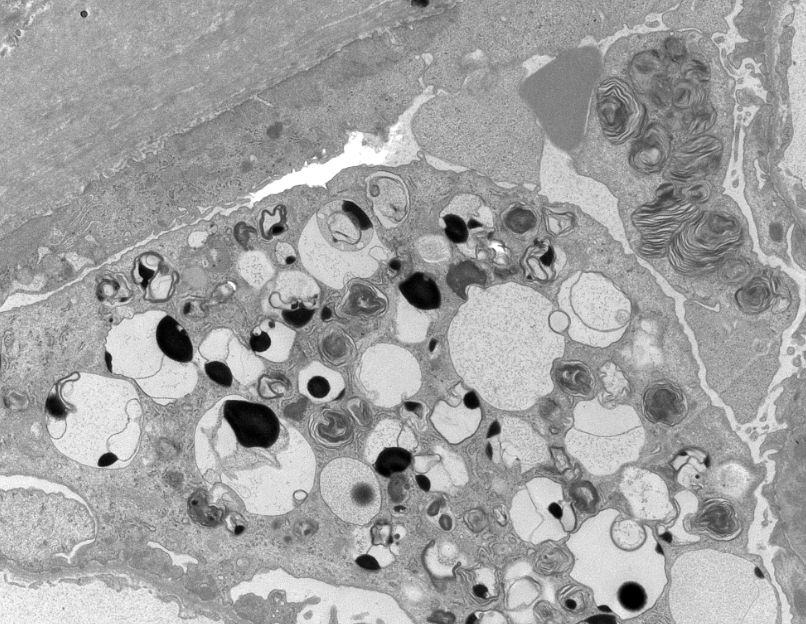
🔹Rare case of secondary renal hemosiderosis after valve surgery
🔹Beautiful histology, Prussian blue, and EM images showing hemosiderin deposit
#MedSky #NephSky @umontreal-en.bsky.social

doi.org/10.1016/j.kint.2025.05.033
🔹Rare case of secondary renal hemosiderosis after valve surgery
🔹Beautiful histology, Prussian blue, and EM images showing hemosiderin deposit
#MedSky #NephSky @umontreal-en.bsky.social




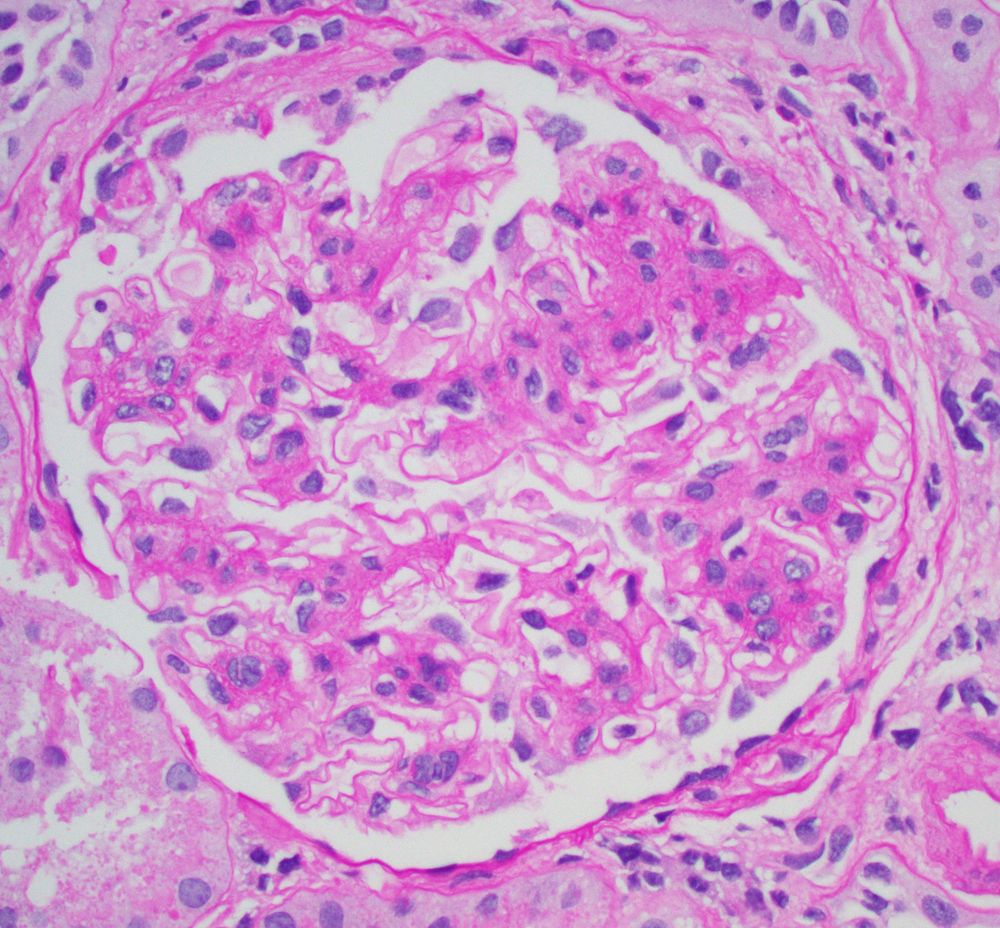
Clues:
- Heavy but focal tubulointerstitial inflammation
- Increased plasma cells
- Viral cytopathic change
- Features of CNI toxicity ->over immunosuppression (isometric vacuolization shown here)
-SV40 IHC confirmatory
#renalpath #pathsky #nephsky




Clues:
- Heavy but focal tubulointerstitial inflammation
- Increased plasma cells
- Viral cytopathic change
- Features of CNI toxicity ->over immunosuppression (isometric vacuolization shown here)
-SV40 IHC confirmatory
#renalpath #pathsky #nephsky

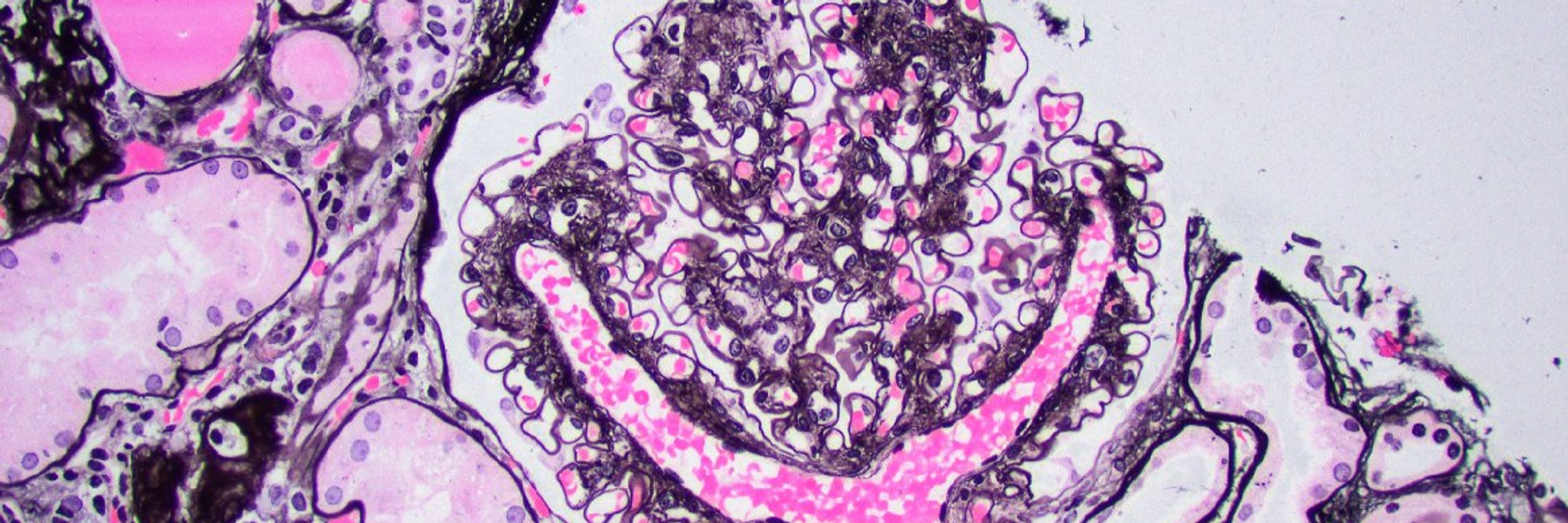
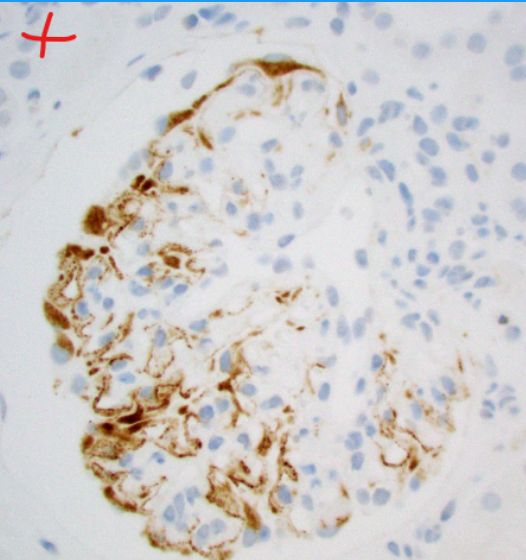
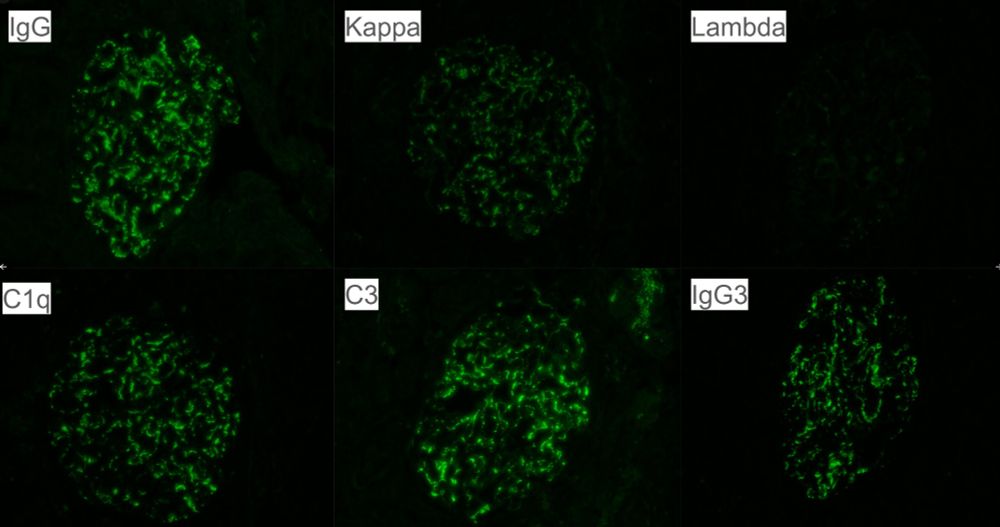
*Glomerulitis (shown in image)
*Transplant glomerulopathy (shown in image)
*Peritubular capillaritis
*Diffuse C4d+ in PTCs on IF
#renalpath #transplant #pathsky #nephsky #medsky

*Glomerulitis (shown in image)
*Transplant glomerulopathy (shown in image)
*Peritubular capillaritis
*Diffuse C4d+ in PTCs on IF
#renalpath #transplant #pathsky #nephsky #medsky










We’re excited to share the moments that shape our residents -
from the microscope to mentorship, and everything in between.
Watch the full video ➨ youtu.be/Yfw39_U9_Hg
#pathology #PathSky #PathMatch26 #PathMatch #Match2026

We’re excited to share the moments that shape our residents -
from the microscope to mentorship, and everything in between.
Watch the full video ➨ youtu.be/Yfw39_U9_Hg
#pathology #PathSky #PathMatch26 #PathMatch #Match2026


















Join our team today! ➨ bit.ly/46CqsrU
Join our team today! ➨ bit.ly/46CqsrU