Arthur Le Coz
@arthurlecoz.bsky.social
54 followers
46 following
13 posts
PhD Candidate in the Dream Team | Paris Brain Institute | Exploring the brain signature and consequences of sleepiness and mental fatigue
Posts
Media
Videos
Starter Packs
Arthur Le Coz
@arthurlecoz.bsky.social
· May 28
Arthur Le Coz
@arthurlecoz.bsky.social
· May 28

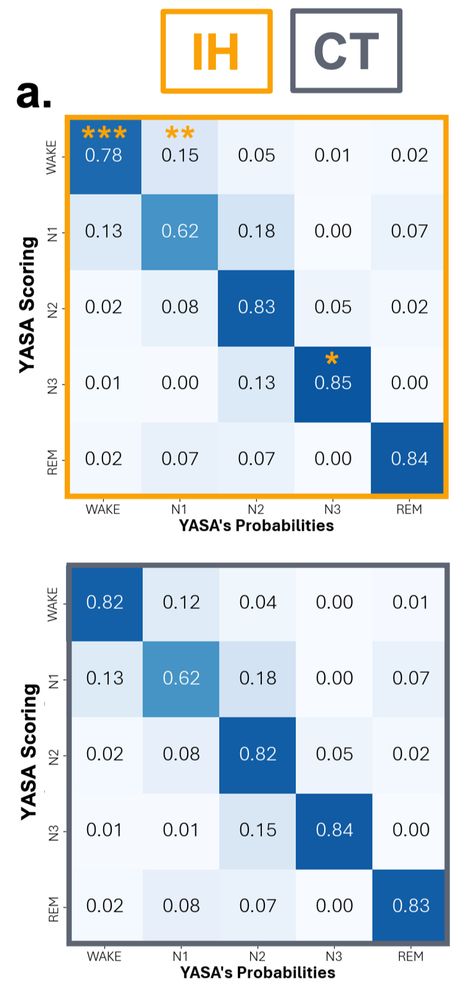
EEG Signature of Idiopathic Hypersomnia: Insights from Sleep Microarchitecture and Hypnodensity Metrics
Background and Objectives: Patients with idiopathic hypersomnia with long sleep time (IH) report daytime hypersomnolence despite prolonged sleep time and normal sleep macrostructure. As they often hav...
www.biorxiv.org
Arthur Le Coz
@arthurlecoz.bsky.social
· May 28
Arthur Le Coz
@arthurlecoz.bsky.social
· May 28
Thomas Andrillon (@thomasandrillon.bsky.social)
In 1/3 of #insomnia, the #1 #sleep disorder, objective sleep recordings do not reveal abnormalities, contradicting subjective assessments.
This has bugged sleep experts for decades!
@rherzoga.bsky.s...
shorturl.at