
🔬 Markus Skrifvars explores its impact:
✅ Higher PaO₂ & lower PaCO₂ with no pressure differences
❓ Key question: Are pneumothorax findings relevant to humans, or is this an effect seen only in pigs? 🐷

🔬 Markus Skrifvars explores its impact:
✅ Higher PaO₂ & lower PaCO₂ with no pressure differences
❓ Key question: Are pneumothorax findings relevant to humans, or is this an effect seen only in pigs? 🐷
🔥 Ari Moskowitz highlights ongoing debates:
🔹 Best device? ETI vs. SGA 🤔
🔹 Video vs. Direct Laryngoscopy 📹
🔹 When to intubate? Timing remains unclear ⏳
🔹 Should strategy vary based on arrest etiology, rhythm, or location?


🔥 Ari Moskowitz highlights ongoing debates:
🔹 Best device? ETI vs. SGA 🤔
🔹 Video vs. Direct Laryngoscopy 📹
🔹 When to intubate? Timing remains unclear ⏳
🔹 Should strategy vary based on arrest etiology, rhythm, or location?
🔥 Ari Moskowitz highlights ongoing debates:
🔹 Best device? ETI vs. SGA 🤔
🔹 Video vs. Direct Laryngoscopy 📹
🔹 When to intubate? Timing remains unclear ⏳
🔹 Should strategy vary based on arrest etiology, rhythm, or location?


🔥 Ari Moskowitz highlights ongoing debates:
🔹 Best device? ETI vs. SGA 🤔
🔹 Video vs. Direct Laryngoscopy 📹
🔹 When to intubate? Timing remains unclear ⏳
🔹 Should strategy vary based on arrest etiology, rhythm, or location?
🔹 OHCA: RCTs suggest SGA may be as good or better than ETI, based on operator skill.
🔹 IHCA: Limited data—observational studies lean toward no intubation
🔹 Ongoing trials comparing SGA vs. ETI for IHCA.

🔹 OHCA: RCTs suggest SGA may be as good or better than ETI, based on operator skill.
🔹 IHCA: Limited data—observational studies lean toward no intubation
🔹 Ongoing trials comparing SGA vs. ETI for IHCA.
📢 Markus Skrifvars on why IV remains the first choice:
✅ Higher ROSC rate
✅ Standard method for non-cardiac arrest patients
✅ As fast as IO in most cases
✅ Less expensive

📢 Markus Skrifvars on why IV remains the first choice:
✅ Higher ROSC rate
✅ Standard method for non-cardiac arrest patients
✅ As fast as IO in most cases
✅ Less expensive
🔍 Markus Skrifvars explores the pros & cons:
✅ IO is as good as IV—but not better
💰 More expensive & should be second choice after IV
🚑 Useful in EMS for patients with difficult access (e.g., children)
⚡ No faster than IV

🔍 Markus Skrifvars explores the pros & cons:
✅ IO is as good as IV—but not better
💰 More expensive & should be second choice after IV
🚑 Useful in EMS for patients with difficult access (e.g., children)
⚡ No faster than IV
📢 Sharon Einav presents the methodology & PICO questions shaping the upcoming recommendations.
🔹 Evidence-based updates coming in the next few months!
🔹 Focus on best practices for managing cardiac arrest in surgical patients.

📢 Sharon Einav presents the methodology & PICO questions shaping the upcoming recommendations.
🔹 Evidence-based updates coming in the next few months!
🔹 Focus on best practices for managing cardiac arrest in surgical patients.
Moderated by Michel Slama & @fabio_taccone, this session dives into the latest advances in cardiopulmonary resuscitation

Moderated by Michel Slama & @fabio_taccone, this session dives into the latest advances in cardiopulmonary resuscitation
👏 Xavier Monnet presents this year’s best research contributions!
📊 431 abstracts submitted
✅ 321 abstracts accepted
🏅 4 awards + 1 ISF (International Sepsis Forum) award
A celebration of innovation and excellence in intensive care research!

👏 Xavier Monnet presents this year’s best research contributions!
📊 431 abstracts submitted
✅ 321 abstracts accepted
🏅 4 awards + 1 ISF (International Sepsis Forum) award
A celebration of innovation and excellence in intensive care research!
📊 Thousands of patients, consistent data, and mortality reduction, yet SDD remains underutilized.
🔹 Open questions:
•Availability
•Optimal regimen
•Impact on microbiome
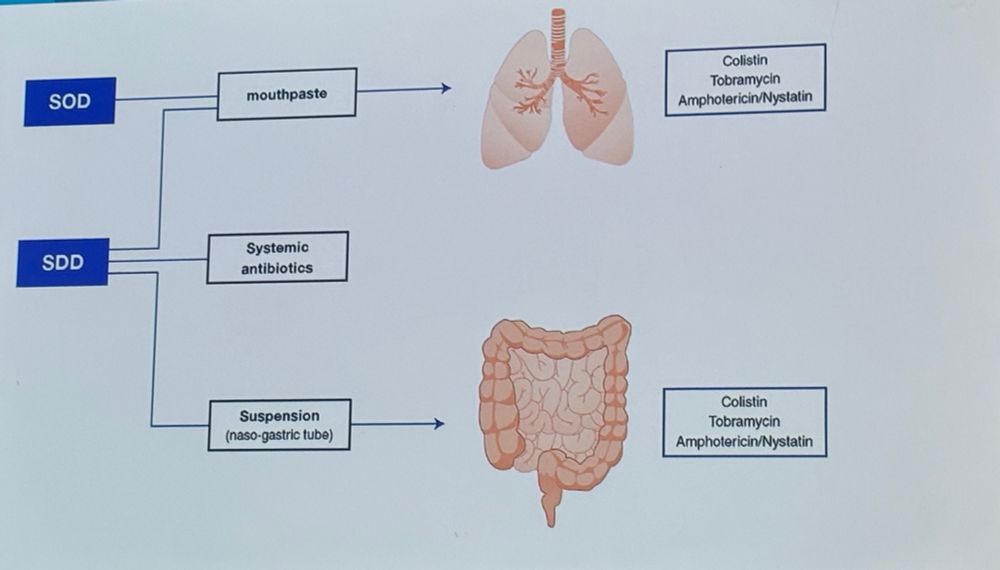
📊 Thousands of patients, consistent data, and mortality reduction, yet SDD remains underutilized.
🔹 Open questions:
•Availability
•Optimal regimen
•Impact on microbiome
🔹 19% of patients had antibiotics reinitiated frequently
Reinitiating antibiotics is linked to:
📈 Longer ICU stay (22.0 vs. 15.9 days)
⚠️ Higher 90-day mortality (40% vs. 25%)

🔹 19% of patients had antibiotics reinitiated frequently
Reinitiating antibiotics is linked to:
📈 Longer ICU stay (22.0 vs. 15.9 days)
⚠️ Higher 90-day mortality (40% vs. 25%)
🔹 Outpatients: ≤5 days if stable
🔹 Non-severe inpatients: <5 days (minimum 3)
🔹 Severe CAP: ≥5 days if stable
Key question: Can clinical stability criteria from CAP be applied to SCAP patients on mechanical ventilation?
🔹 Outpatients: ≤5 days if stable
🔹 Non-severe inpatients: <5 days (minimum 3)
🔹 Severe CAP: ≥5 days if stable
Key question: Can clinical stability criteria from CAP be applied to SCAP patients on mechanical ventilation?
📊 Evolution to visual decision support tools
🔹 Turning data into knowledge
⚡ Faster & more accurate detection of abnormalities
🧠 Improving situation awareness & reducing cognitive workload

📊 Evolution to visual decision support tools
🔹 Turning data into knowledge
⚡ Faster & more accurate detection of abnormalities
🧠 Improving situation awareness & reducing cognitive workload
🔹 New ways to display monitoring variables
🔹 Advanced tools to visualize data
🔹 Seamless data integration into a single monitor
🔹 Data fusion—combining variables into one visual tool

🔹 New ways to display monitoring variables
🔹 Advanced tools to visualize data
🔹 Seamless data integration into a single monitor
🔹 Data fusion—combining variables into one visual tool
🔹 No perfect detection algorithm exists—manual confirmation is key
🔹 Visual decision support tools enhance clinician feedback
🔹 Real-time compliance reports enable reinforced learning


🔹 No perfect detection algorithm exists—manual confirmation is key
🔹 Visual decision support tools enhance clinician feedback
🔹 Real-time compliance reports enable reinforced learning
🔹 The key to precision resuscitation:
•Is the patient in compensated shock?
•Will cardiac output improve with fluids?
•What is the arterial tone status?
•Can the heart sustain output without filling pressures?

🔹 The key to precision resuscitation:
•Is the patient in compensated shock?
•Will cardiac output improve with fluids?
•What is the arterial tone status?
•Can the heart sustain output without filling pressures?
🔹 Stepwise decision-making:
✅ Is the patient hemodynamically stable? If yes, do nothing.
✅ If unstable, assess preload responsiveness.
✅ If preload-responsive, evaluate vasomotor tone


🔹 Stepwise decision-making:
✅ Is the patient hemodynamically stable? If yes, do nothing.
✅ If unstable, assess preload responsiveness.
✅ If preload-responsive, evaluate vasomotor tone
✅ Guided resuscitation with clear decision rules
✅ Standardized yet personalized fluid & vasopressor strategies
✅ Adaptable across ICUs, remote care, and austere environments
Looking at the future!

✅ Guided resuscitation with clear decision rules
✅ Standardized yet personalized fluid & vasopressor strategies
✅ Adaptable across ICUs, remote care, and austere environments
Looking at the future!
🚀 Moving beyond syndromes to treatable traits
🔹 Reframing immunobiology for better-targeted therapies
🎯 Immune modulation: precision over generalization
🧬 Metabolic reprogramming—a new frontier?


🚀 Moving beyond syndromes to treatable traits
🔹 Reframing immunobiology for better-targeted therapies
🎯 Immune modulation: precision over generalization
🧬 Metabolic reprogramming—a new frontier?
"The conclusion is quite simple: If you think measuring pupils makes sense, the pupillometer is better than you!"
🔹 Objective, reproducible, and precise
🔹 Eliminates subjectivity in pupil assessment


"The conclusion is quite simple: If you think measuring pupils makes sense, the pupillometer is better than you!"
🔹 Objective, reproducible, and precise
🔹 Eliminates subjectivity in pupil assessment
🔹 Increase mobility & physical therapy
🔹 Reduce invasive devices & sampling
🔹 Improve data visualization & reduce fatigue
🔹 Detect delirium earlier
🔹 Bridge monitoring gaps between ICU & wards


🔹 Increase mobility & physical therapy
🔹 Reduce invasive devices & sampling
🔹 Improve data visualization & reduce fatigue
🔹 Detect delirium earlier
🔹 Bridge monitoring gaps between ICU & wards

After the first fluid challenge in septic shock, BP rises from 90/40 to 95/45. What’s the next move?
More fluids 💧 or start vasopressors 💉

After the first fluid challenge in septic shock, BP rises from 90/40 to 95/45. What’s the next move?
More fluids 💧 or start vasopressors 💉
🗣️ Moderator: Xavier Monnet
💡 Experts: Daniel De Backer, Emily J See, Jean-Louis Teboul, Michelle Chew

🗣️ Moderator: Xavier Monnet
💡 Experts: Daniel De Backer, Emily J See, Jean-Louis Teboul, Michelle Chew



