Edition-2: Artificial Intelligence (AI) in Medicine – AIIM 2026
May 04–05, 2026
Boston, Massachusetts, USA
🌐 ai-medicalcongress.com
#AIIM2026 #AIinMedicine #MedicalAI #DigitalHealth #ClinicalDecisionSupport #WearableAI #HealthcareInnovation

Edition-2: Artificial Intelligence (AI) in Medicine – AIIM 2026
May 04–05, 2026
Boston, Massachusetts, USA
🌐 ai-medicalcongress.com
#AIIM2026 #AIinMedicine #MedicalAI #DigitalHealth #ClinicalDecisionSupport #WearableAI #HealthcareInnovation


E. C. d., J. G. V. d. et al.
Paper
Details
#ClinicalDecisionSupport #PhysicianPractice #HealthTechResearch
E. C. d., J. G. V. d. et al.
Paper
Details
#ClinicalDecisionSupport #PhysicianPractice #HealthTechResearch
www.thieme-connect.de/products/ejo...
#MedSky #CDS #DigitalHealth

www.thieme-connect.de/products/ejo...
#MedSky #CDS #DigitalHealth
#MedSky #CDS #PalliativeCare #DigitalHealth

#MedSky #CDS #PalliativeCare #DigitalHealth
www.sciencedirect.com/science/arti...
#IDSky #IDSkyFr #InfectiousDiseases #AI #GenerativeArtificialIntelligence #MachineLearning #ClinicalDecisionSupport
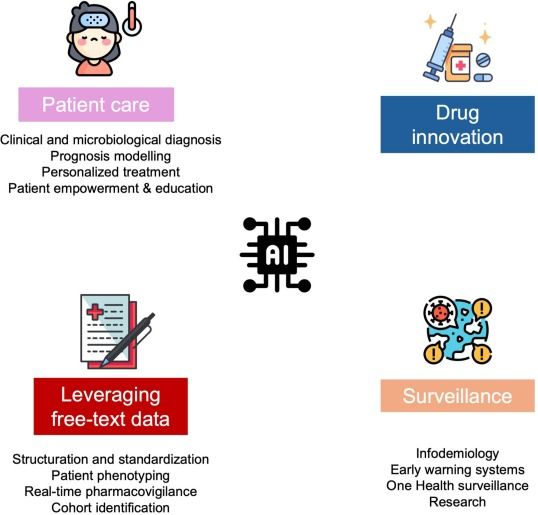
www.sciencedirect.com/science/arti...
#IDSky #IDSkyFr #InfectiousDiseases #AI #GenerativeArtificialIntelligence #MachineLearning #ClinicalDecisionSupport
Learn more and request a demo at re.doctor.
#VitalSigns #PatientMonitoring

Learn more and request a demo at re.doctor.
#VitalSigns #PatientMonitoring


Read the full article at the "News & Press" #LinkInBio.
#Cancer #ClinicalDecisionSupport #PrecisionMedicine

Read the full article at the "News & Press" #LinkInBio.
#Cancer #ClinicalDecisionSupport #PrecisionMedicine

#MedSky #CDS #ClinicalDecisionSupport #DigitalHealth

#MedSky #CDS #ClinicalDecisionSupport #DigitalHealth
#MedSky #CDS #DigitalHealth #ClinicalDecisionSupport @mozkaynak.bsky.social

#MedSky #CDS #DigitalHealth #ClinicalDecisionSupport @mozkaynak.bsky.social
Hear what Dr. Peter Kaufman, Oncologist at the University of Vermont Cancer Center, had to say about Oncoscope Edge: bit.ly/41LEK6U
#Oncology #ClinicalDecisionSupport #PrecisionMedicine

Hear what Dr. Peter Kaufman, Oncologist at the University of Vermont Cancer Center, had to say about Oncoscope Edge: bit.ly/41LEK6U
#Oncology #ClinicalDecisionSupport #PrecisionMedicine

#MedSky #CDS #DigitalHealth

#MedSky #CDS #DigitalHealth

Caceres, J., Chavez-Lencinas, C. et al.
Paper
Details
#OneChoiceAI #ClinicalDecisionSupport #BacteremiaTreatmentPeru
Caceres, J., Chavez-Lencinas, C. et al.
Paper
Details
#OneChoiceAI #ClinicalDecisionSupport #BacteremiaTreatmentPeru

www.sciencedirect.com/science/arti...
#IDsky #InfectiousDiseases #ArtificialIntelligence #GenerativeArtificialIntelligence #MachineLearning #ClinicalDecisionSupport

www.sciencedirect.com/science/arti...
#IDsky #InfectiousDiseases #ArtificialIntelligence #GenerativeArtificialIntelligence #MachineLearning #ClinicalDecisionSupport
venturevalkyrie.com/ai-large-lan...
venturevalkyrie.com/ai-large-lan...
But patients rarely have the opportunity to trial different options. Caplex™️ changes that.
Experience multiple options in a single session—and walk away with the one that works best for them.
🔗 humotech.com/clinical/
#ClinicalDecisionSupport

But patients rarely have the opportunity to trial different options. Caplex™️ changes that.
Experience multiple options in a single session—and walk away with the one that works best for them.
🔗 humotech.com/clinical/
#ClinicalDecisionSupport
#PERMANENS #IASP2025 #MentalHealth #SuicidePrevention #ClinicalDecisionSupport #SelfHarm #DigitalHealth #EmergencyCare
#PERMANENS #IASP2025 #MentalHealth #SuicidePrevention #ClinicalDecisionSupport #SelfHarm #DigitalHealth #EmergencyCare

