Tony Breu
@tonybreu.bsky.social
2.9K followers
150 following
3K posts
Hospitalist, VA Boston Healthcare System. Co-host, Curious Clinicians Podcast
Posts
Media
Videos
Starter Packs
Reposted by Tony Breu
Tony Breu
@tonybreu.bsky.social
· Nov 28
Reposted by Tony Breu
Tony Breu
@tonybreu.bsky.social
· Nov 28
Reposted by Tony Breu
Reposted by Tony Breu
Reposted by Tony Breu
Tony Breu
@tonybreu.bsky.social
· Nov 28
Tony Breu
@tonybreu.bsky.social
· Nov 28
Tony Breu
@tonybreu.bsky.social
· Nov 23
Tony Breu
@tonybreu.bsky.social
· Nov 22
Reposted by Tony Breu
Rahul Ganatra
@rbganatra.bsky.social
· Nov 22
Albumin for Spontaneous Bacterial Peritonitis: Care... : Official journal of the American College of Gastroenterology | ACG
ated trends and patient, practice-, and facility-level factors associated with use among patients with cirrhosis hospitalized for SBP confirmed with ascitic fluid criteria.
Results:
Among 3,871 Vet...
journals.lww.com
Tony Breu
@tonybreu.bsky.social
· Nov 21
Reposted by Tony Breu
Reposted by Tony Breu
Joel Topf
@kidneyboy.bsky.social
· Nov 19
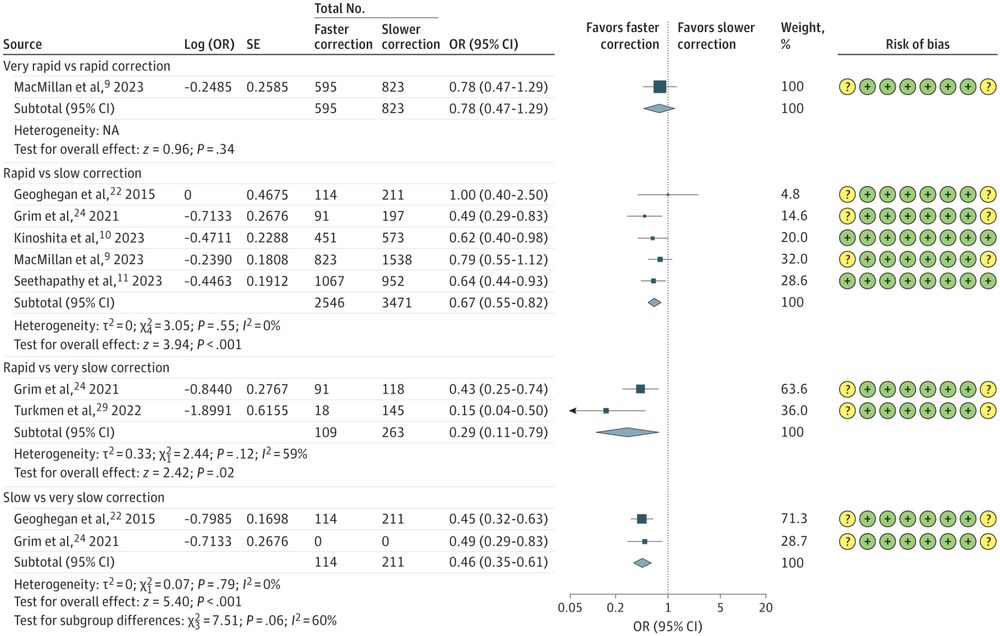
Correction Rates and Clinical Outcomes in Hospitalized Adults With Severe Hyponatremia
This systematic review and meta-analysis evaluates the association of sodium correction rates with mortality among hospitalized adults with severe hyponatremia.
jamanetwork.com