References📄:
1. bit.ly/3RdSnpA
2. bit.ly/3FKSRky
3. bit.ly/4bxcAQR, bit.ly/42bmcgR
4. bit.ly/4iBxnoH, bit.ly/4hEie4T

References📄:
1. bit.ly/3RdSnpA
2. bit.ly/3FKSRky
3. bit.ly/4bxcAQR, bit.ly/42bmcgR
4. bit.ly/4iBxnoH, bit.ly/4hEie4T
Q5: What are some of the latest advancements in the treatment of hereditary colorectal cancer syndromes?
#Gastrosky
Q5: What are some of the latest advancements in the treatment of hereditary colorectal cancer syndromes?
#Gastrosky
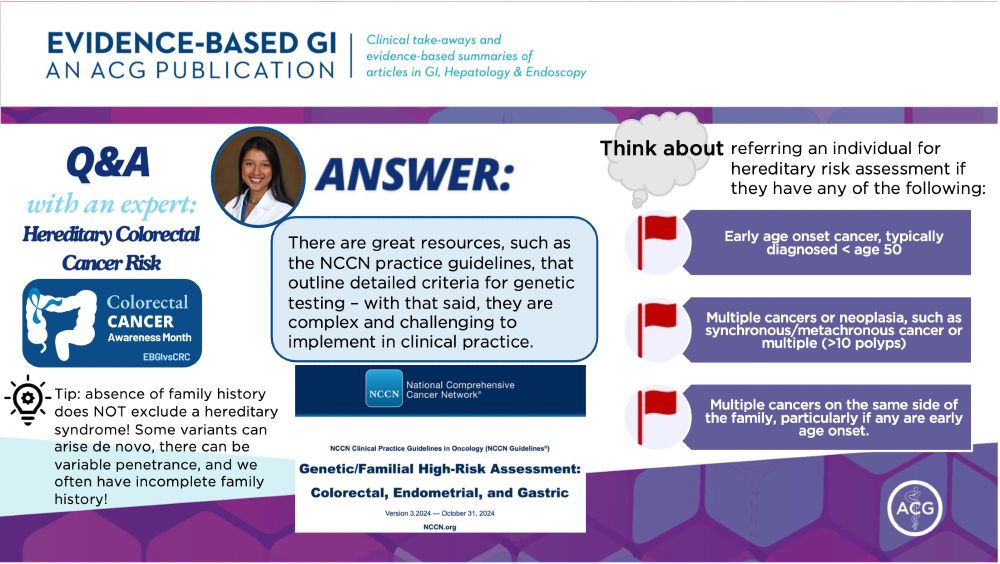
VUS: genetic alteration w/ unknown disease risk
🧬 Common, found in 30-50% of patients undergoing multigene panel testing
🧬 >90% of VUS are re-classified as benign over ⏰
⚠️ Do 🚫 recommend changing medical management based on VUS alone!
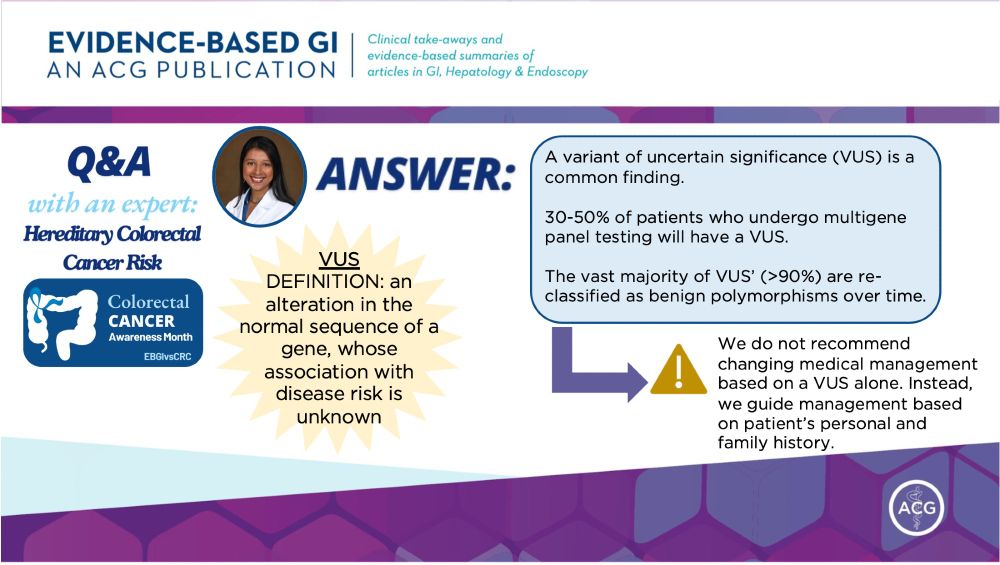
VUS: genetic alteration w/ unknown disease risk
🧬 Common, found in 30-50% of patients undergoing multigene panel testing
🧬 >90% of VUS are re-classified as benign over ⏰
⚠️ Do 🚫 recommend changing medical management based on VUS alone!
Q4: What are the implications of identifying a ”variant of uncertain significance” on genetic testing🧬?
#Gastrosky
Q4: What are the implications of identifying a ”variant of uncertain significance” on genetic testing🧬?
#Gastrosky
NCCN guidelines excellent but complex 👇🏽
bit.ly/4iQwTei
Broadly speaking, think about referring if:
🔎 Early onset cancer age < 50
🔎 Multiple cancers or >10 polyps
🔎 Multiple cancers on same side of family
Note: absence of family hx does not 🚫 a hereditary syndrome!
NCCN guidelines excellent but complex 👇🏽
bit.ly/4iQwTei
Broadly speaking, think about referring if:
🔎 Early onset cancer age < 50
🔎 Multiple cancers or >10 polyps
🔎 Multiple cancers on same side of family
Note: absence of family hx does not 🚫 a hereditary syndrome!
Q3: In what clinical scenarios should gastroenterology providers think about referring patients for genetic testing🧬?
#Gastrosky
Q3: In what clinical scenarios should gastroenterology providers think about referring patients for genetic testing🧬?
#Gastrosky
📝Simple 3Q screening tool (Kastrinos et al. 2009) is feasible!
1. FDR < 50 with CRC, CA of uterus, ovary, stomach, small intestine, urinary tract, bile duct, pancreas, brain?
2. CRC or polyps at age < 50?
3. 3+ relatives w/ CRC?
✅High sensitivity
✅Supported by MSTF on CRC
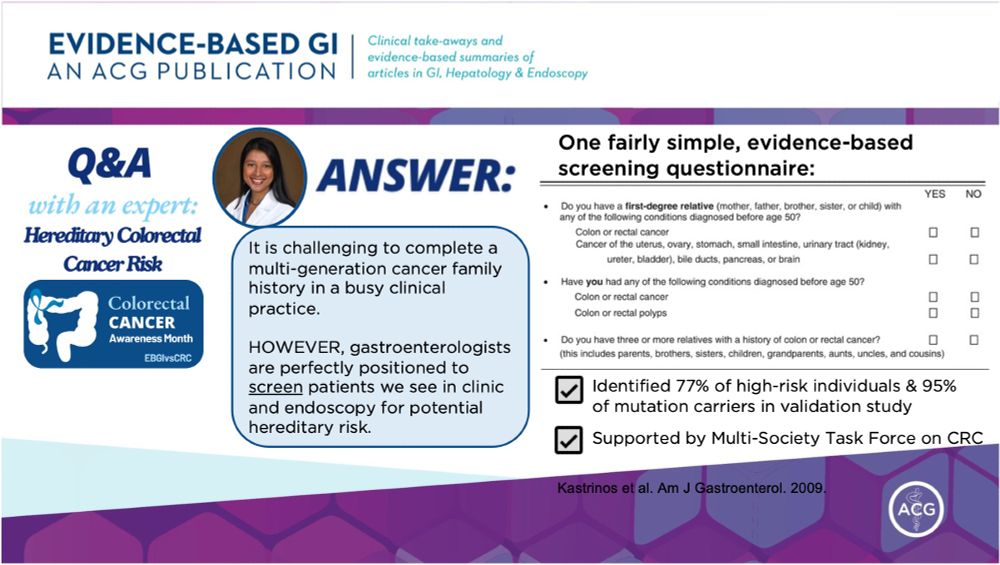
📝Simple 3Q screening tool (Kastrinos et al. 2009) is feasible!
1. FDR < 50 with CRC, CA of uterus, ovary, stomach, small intestine, urinary tract, bile duct, pancreas, brain?
2. CRC or polyps at age < 50?
3. 3+ relatives w/ CRC?
✅High sensitivity
✅Supported by MSTF on CRC
Q2: What are the key elements of a family history that should be collected to assess the risk of hereditary colorectal cancer?
#Gastrosky
Q2: What are the key elements of a family history that should be collected to assess the risk of hereditary colorectal cancer?
#Gastrosky
Hereditary CRC makes up:
🔹10% of all CRC
🔹16% of all CRC in age < 50
Most common: Lynch syndrome
Caused by:
🧬MMR gene mutations including MLH1, MSH2, MSH6, PMS2
or
🧬EPCAM mutation which sits upstream of MSH2)
Prevalence: 1/279 individuals in general population👥
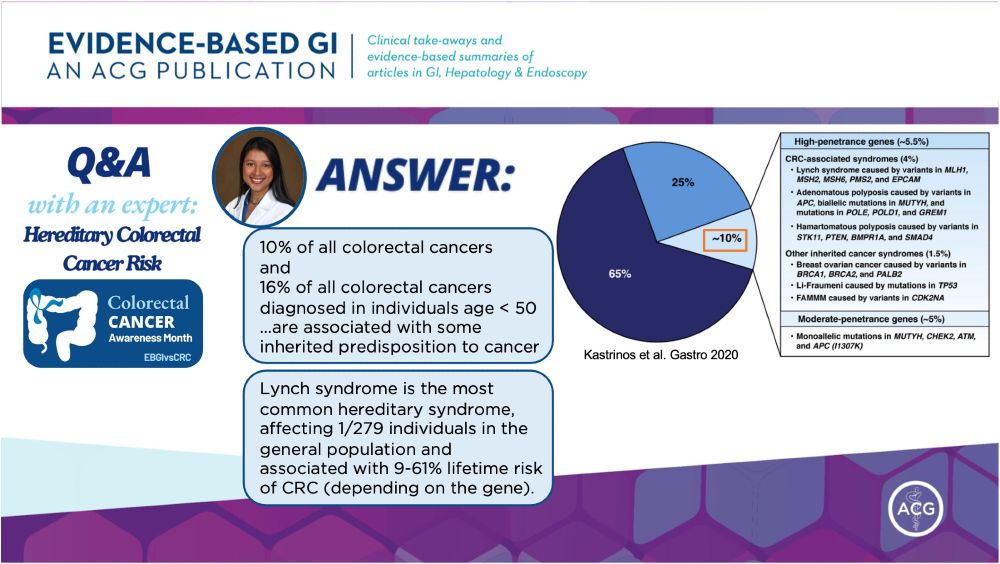
Hereditary CRC makes up:
🔹10% of all CRC
🔹16% of all CRC in age < 50
Most common: Lynch syndrome
Caused by:
🧬MMR gene mutations including MLH1, MSH2, MSH6, PMS2
or
🧬EPCAM mutation which sits upstream of MSH2)
Prevalence: 1/279 individuals in general population👥