
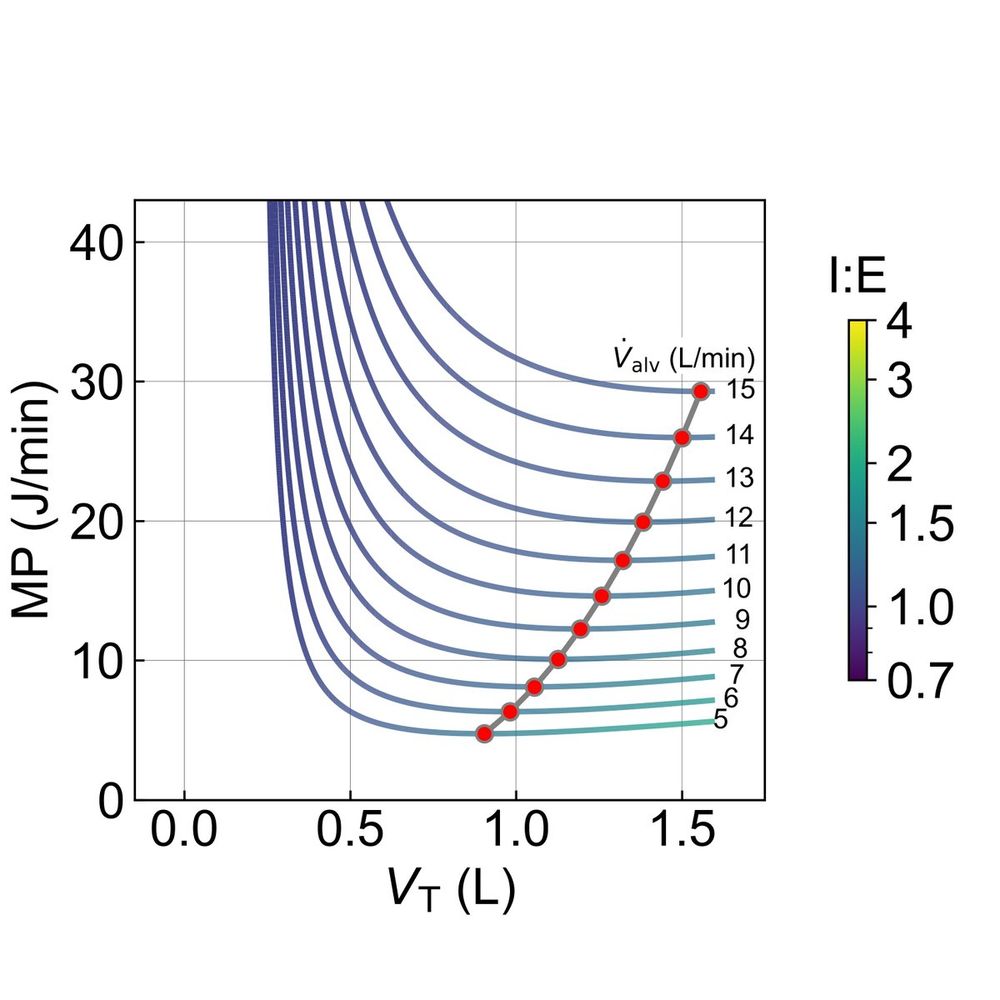
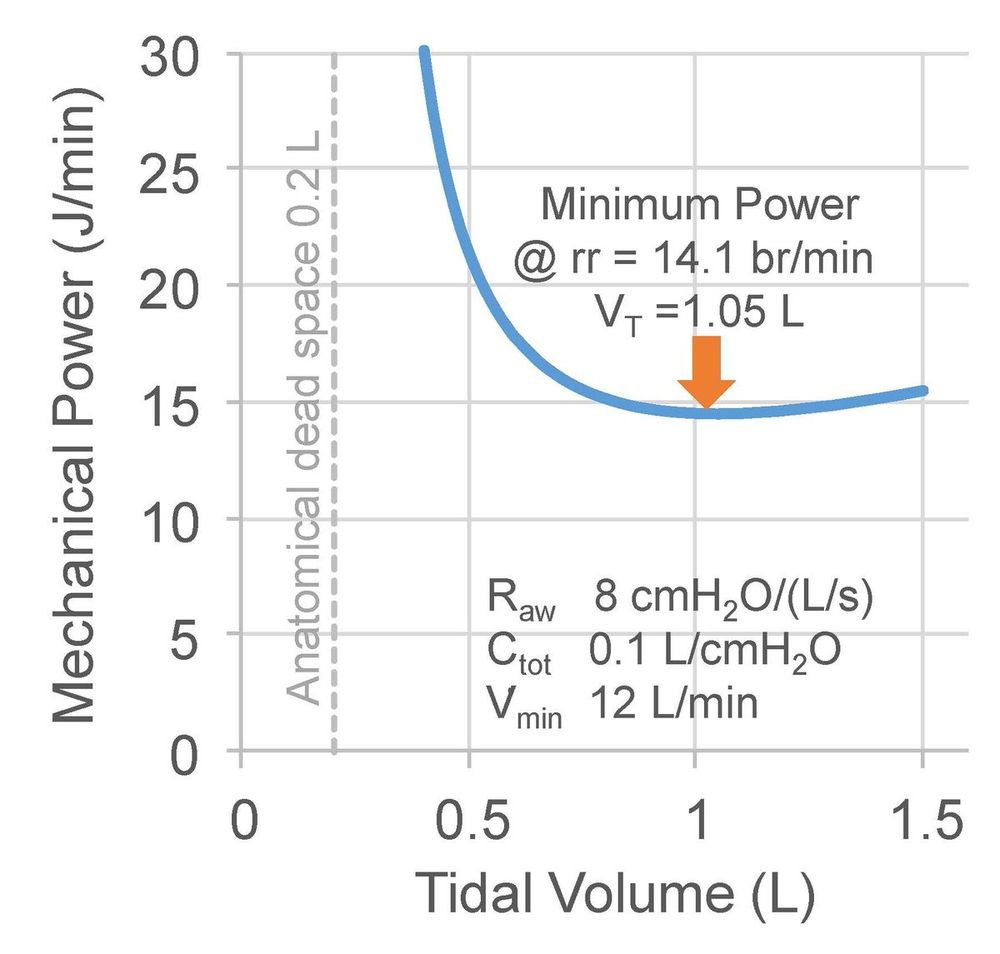
For any given V'min, a tidal volume of twice the anatomic dead space (~4.4 ml/kg in adults) always minimizes elastic mechanical power (the energy needed for lung expansion).
medrxiv.org/content/10.110…
For any given V'min, a tidal volume of twice the anatomic dead space (~4.4 ml/kg in adults) always minimizes elastic mechanical power (the energy needed for lung expansion).
medrxiv.org/content/10.110…
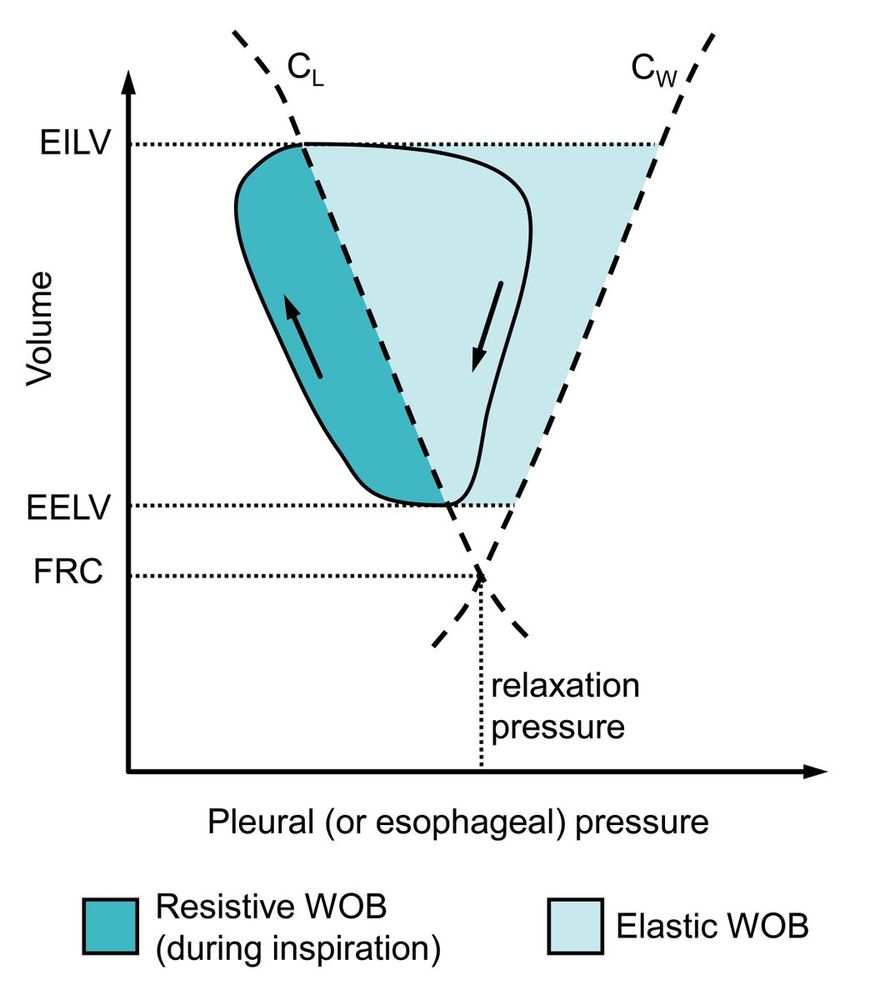
rdcu.be/dU9Nj
rdcu.be/dU9Nj
@gattinon
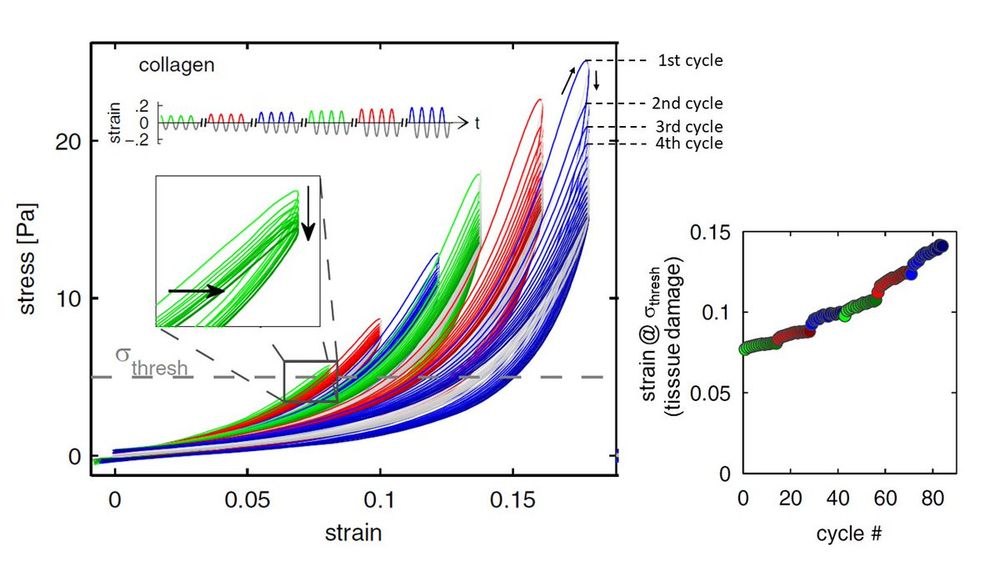
bio.physik.fau.de/publications/M…
@gattinon
bio.physik.fau.de/publications/M…
bit.ly/3HVrsuh
bit.ly/3HVrsuh
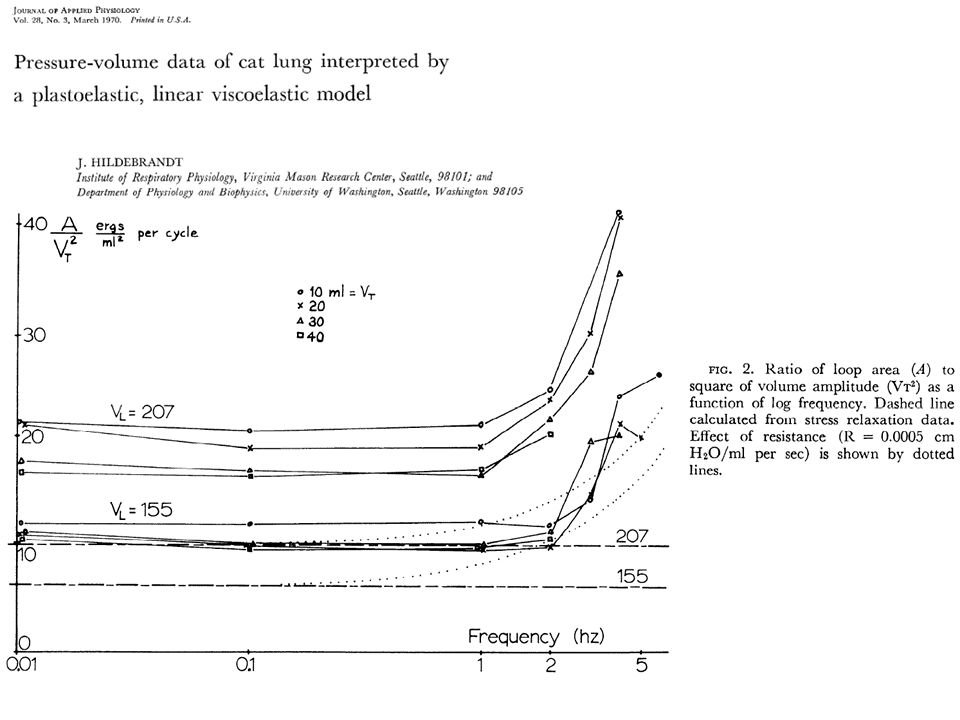











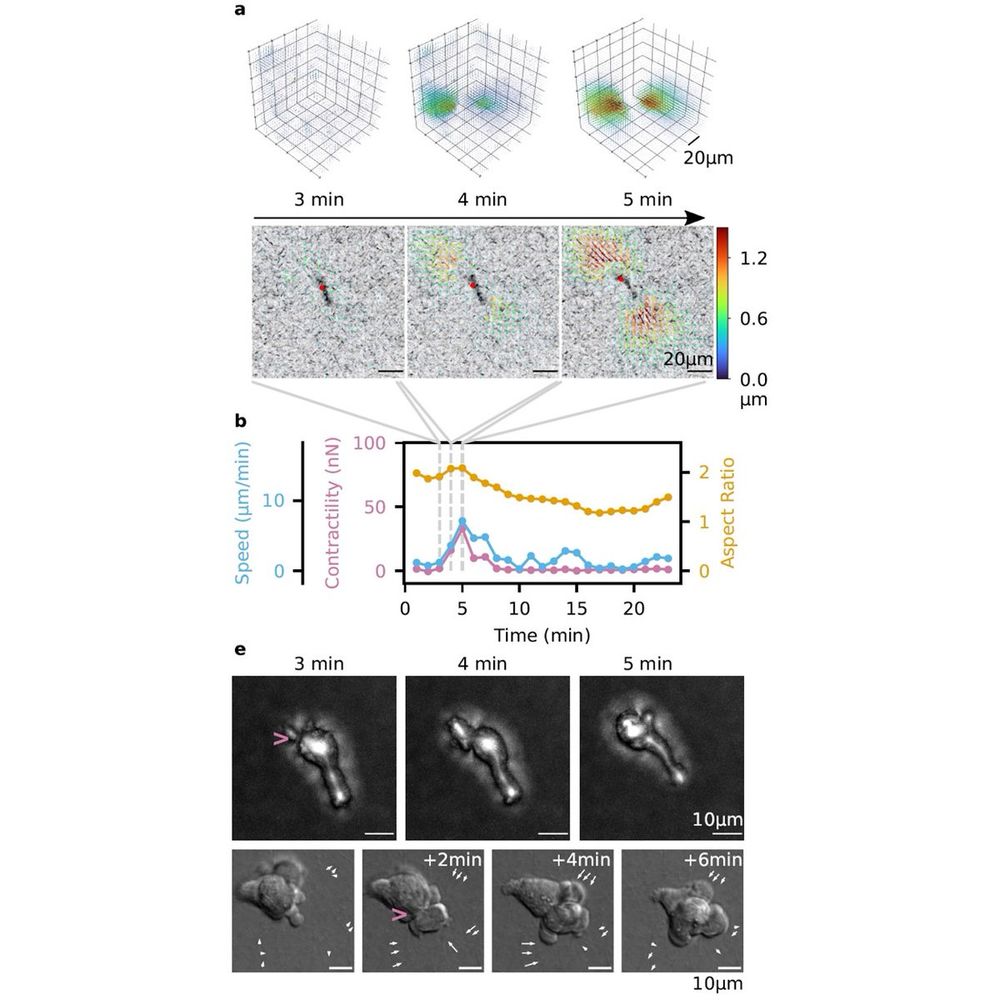
doi.org/10.1088/1758-5…

doi.org/10.1088/1758-5…




