Trouble With MedPAC - WSJ share.google/M9VyVAt9V255...

Trouble With MedPAC - WSJ share.google/M9VyVAt9V255...


www.nber.org/papers/w34791

www.nber.org/papers/w34791
www.nber.org/papers/w34791

www.nber.org/papers/w34791
@jamainternalmed.com @mlbarnett.bsky.social: jamanetwork.com/journals/jam...


@jamainternalmed.com @mlbarnett.bsky.social: jamanetwork.com/journals/jam...


jamanetwork.com/journals/jam...

jamanetwork.com/journals/jam...

In a new paper, we look at how often spend-down happens in nursing homes specifically

In a new paper, we look at how often spend-down happens in nursing homes specifically

Hospitals are complaining across the US that patients are "stuck" waiting for rehab beds at nursing homes when they are medically stable and ready for discharge. What is going on??
jamanetwork.com/journals/jam...

Medicare saves lives. But is it enough to save lives of the most vulnerable Americans? The study suggests no; Medicaid still matters. (1/11)
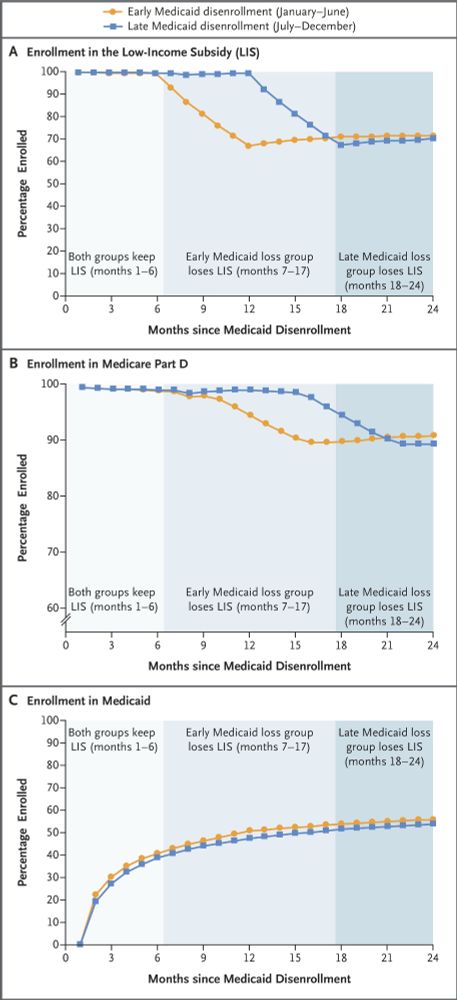
Medicare saves lives. But is it enough to save lives of the most vulnerable Americans? The study suggests no; Medicaid still matters. (1/11)

jobs.academyhealth.org/jobs/view/as...
Happy to chat!
#econsky #policysky
jobs.academyhealth.org/jobs/view/as...
Happy to chat!
#econsky #policysky
In nearly every state, after your initial eligibility period @65, you can't revert to traditional Medicare without facing medical underwriting for Medigap plan that cover your out-of-pocket obligations.
In nearly every state, after your initial eligibility period @65, you can't revert to traditional Medicare without facing medical underwriting for Medigap plan that cover your out-of-pocket obligations.
The so-called "Dual-eligibles".

