Daniel L. Barber, PhD
@danbarberphd.bsky.social
2.3K followers
270 following
9 posts
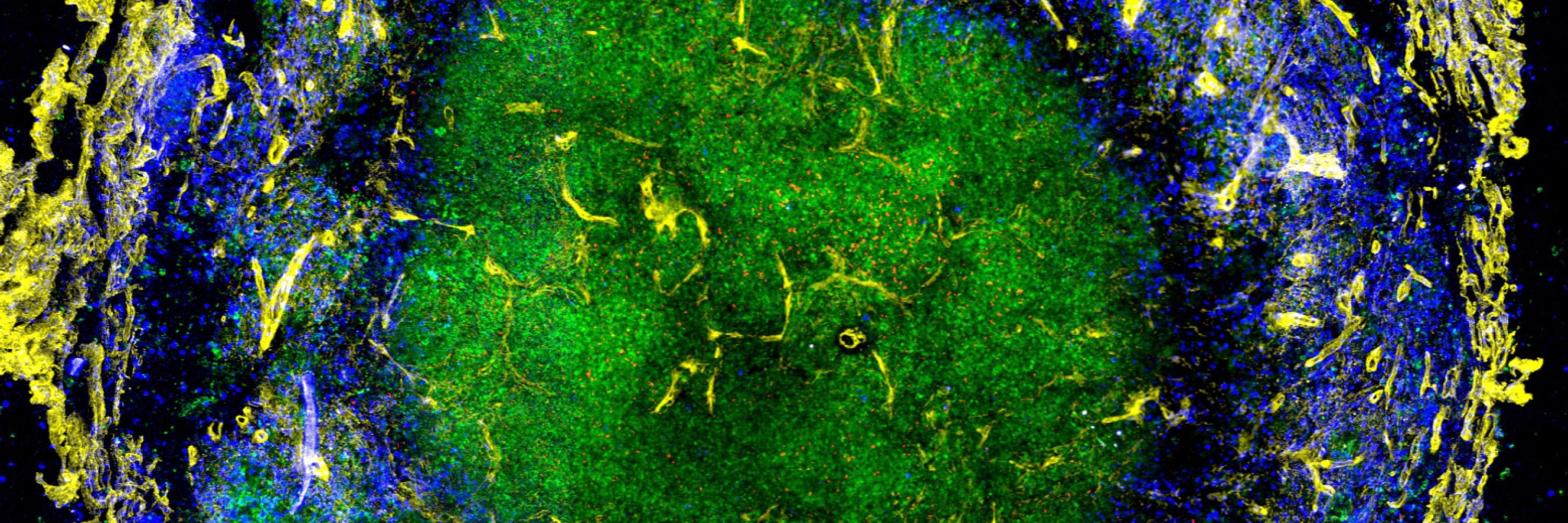
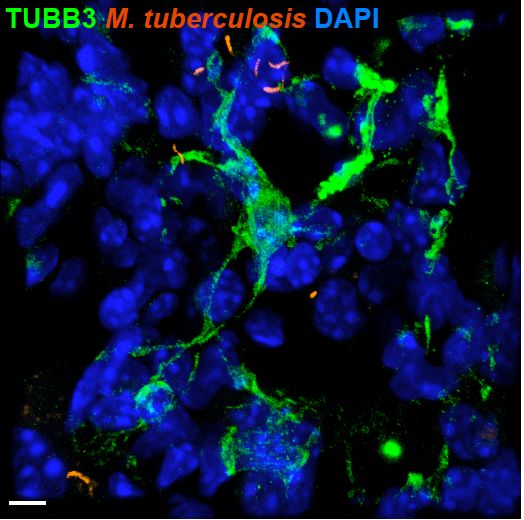
Immunologist. Major focus is on T cell responses to Mycobacterium tuberculosis infection.
Posts
Media
Videos
Starter Packs
Reposted by Daniel L. Barber, PhD
Reposted by Daniel L. Barber, PhD
Reposted by Daniel L. Barber, PhD
Paul Baker
@pauljbaker.bsky.social
· Dec 7
Reposted by Daniel L. Barber, PhD
Paul Baker
@pauljbaker.bsky.social
· Dec 7
Reposted by Daniel L. Barber, PhD
Reposted by Daniel L. Barber, PhD
Reposted by Daniel L. Barber, PhD
Gabriele Pollara
@gpollara.bsky.social
· Nov 11
Reposted by Daniel L. Barber, PhD