José Molina
@josemolinagb.bsky.social
1.6K followers
780 following
150 posts
ID doc & Antibiotic Steward •
• Clinical trials and #FOAMed believer •
Now on @shorten2trial.bsky.social
#AMSsky #IDSky #AMR
Hospital Virgen del Rocío • Seville, Spain 🇪🇸
Posts
Media
Videos
Starter Packs
Pinned
Reposted by José Molina
Reposted by José Molina
Reposted by José Molina
Reposted by José Molina
Reposted by José Molina
José Molina
@josemolinagb.bsky.social
· Jul 20
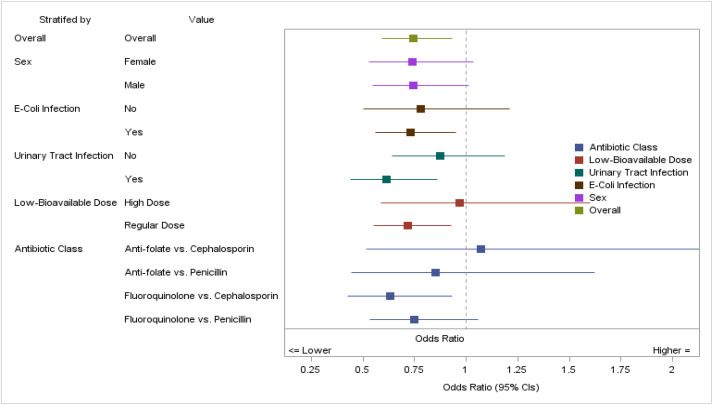
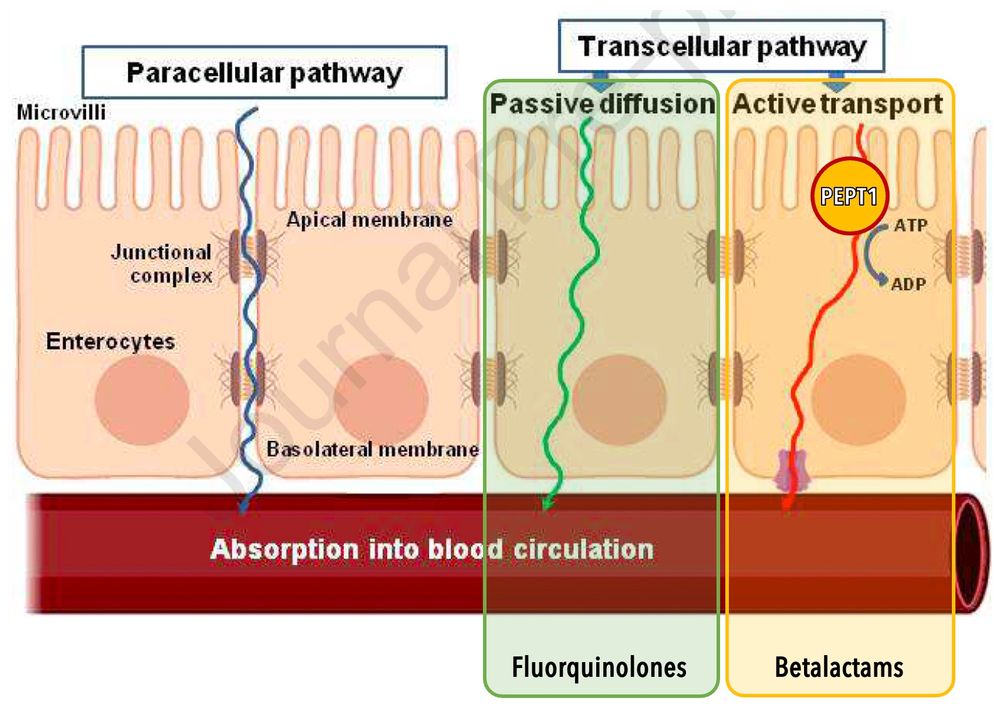
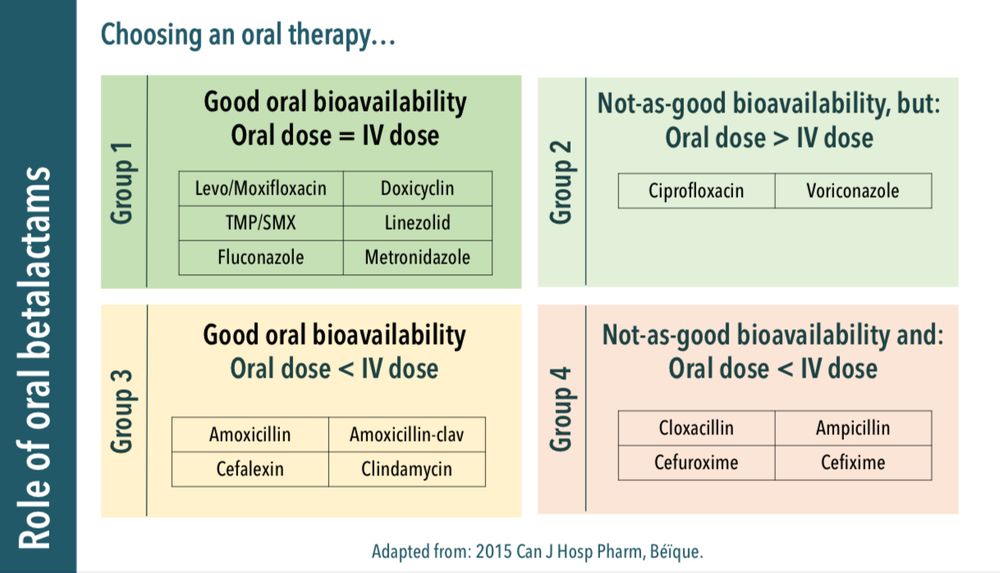
Highly versus less bioavailable oral antibiotics in the treatment of gram-negative bloodstream infections: a propensity-matched cohort analysis
In this study, we evaluated the clinical outcomes associated with the use of highly
bioavailable oral antibiotics (fluoroquinolones and trimethoprim-sulfamethoxazole)
compared with the less-bioavailab...
www.clinicalmicrobiologyandinfection.com
José Molina
@josemolinagb.bsky.social
· Jul 20
José Molina
@josemolinagb.bsky.social
· Jul 20
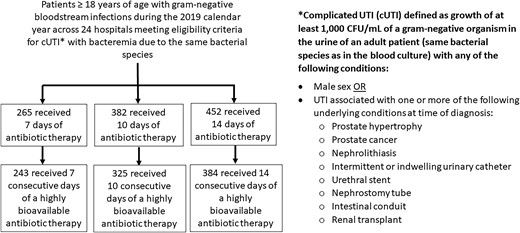
Defining the Optimal Duration of Therapy for Hospitalized Patients With Complicated Urinary Tract Infections and Associated Bacteremia
In a multicenter study of 1099 hospitalized adults with complicated urinary tract infections and associated bacteremia, 7 days of antibiotics was sufficien
academic.oup.com
José Molina
@josemolinagb.bsky.social
· Jul 20
José Molina
@josemolinagb.bsky.social
· Jul 20

Safety of early oral ambulatory treatment of adult patients with bloodstream infections discharged from the emergency department | Antimicrobial Agents and Chemotherapy
Randomized trials have unanimously shown the benefits of oral antibiotic treatments
for stable patients with bacteremia (1). However, transition to oral therapy has been usually performed after severa...
journals.asm.org
José Molina
@josemolinagb.bsky.social
· Jul 20
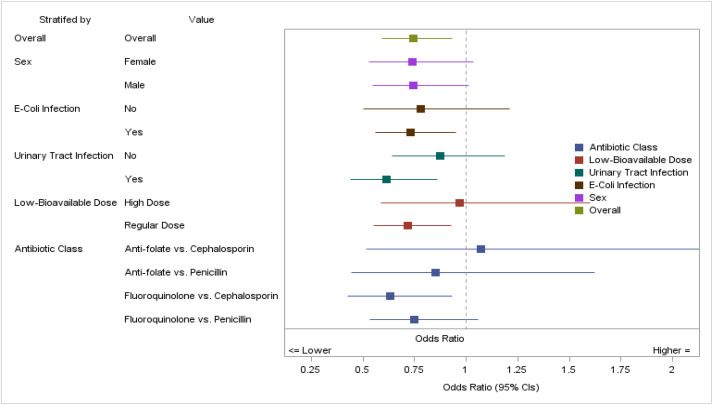
Highly versus less bioavailable oral antibiotics in the treatment of gram-negative bloodstream infections: a propensity-matched cohort analysis
In this study, we evaluated the clinical outcomes associated with the use of highly
bioavailable oral antibiotics (fluoroquinolones and trimethoprim-sulfamethoxazole)
compared with the less-bioavailab...
www.clinicalmicrobiologyandinfection.com
Reposted by José Molina
ID:IOTS Podcast
@idiots-pod.bsky.social
· Jul 20
Reposted by José Molina
Reposted by José Molina
JAC-AMR
@jac-amr.bsky.social
· Jul 18
Reposted by José Molina
Gabriele Pollara
@gpollara.bsky.social
· Jun 30

Pivmecillinam for Treatment of Uncomplicated Urinary Tract Infection: New Efficacy Analysis
This reanalysis of data from historical randomized, controlled trials, according to criteria published by the US Food and Drug Administration in 2019, conf
academic.oup.com
José Molina
@josemolinagb.bsky.social
· Jul 19
Reposted by José Molina
José Molina
@josemolinagb.bsky.social
· Jul 19
José Molina
@josemolinagb.bsky.social
· Nov 12

Safety of early oral ambulatory treatment of adult patients with bloodstream infections discharged from the emergency department | Antimicrobial Agents and Chemotherapy
Randomized trials have unanimously shown the benefits of oral antibiotic treatments for stable patients with bacteremia (1). However, transition to oral therapy has been usually performed after several days of intravenous treatment—frequently up to 7 days (2)—highlighting the need for evidence of the safety of earlier oral treatments (3).
journals.asm.org
José Molina
@josemolinagb.bsky.social
· Jul 19
José Molina
@josemolinagb.bsky.social
· Jul 19
José Molina
@josemolinagb.bsky.social
· Nov 12

Safety of early oral ambulatory treatment of adult patients with bloodstream infections discharged from the emergency department | Antimicrobial Agents and Chemotherapy
Randomized trials have unanimously shown the benefits of oral antibiotic treatments for stable patients with bacteremia (1). However, transition to oral therapy has been usually performed after several days of intravenous treatment—frequently up to 7 days (2)—highlighting the need for evidence of the safety of earlier oral treatments (3).
journals.asm.org